Hypothyroidism is a disorder of the endocrine system in which the thyroid gland doesn’t create and release enough thyroid hormone to meet the body’s needs. Also known as underactive thyroid.
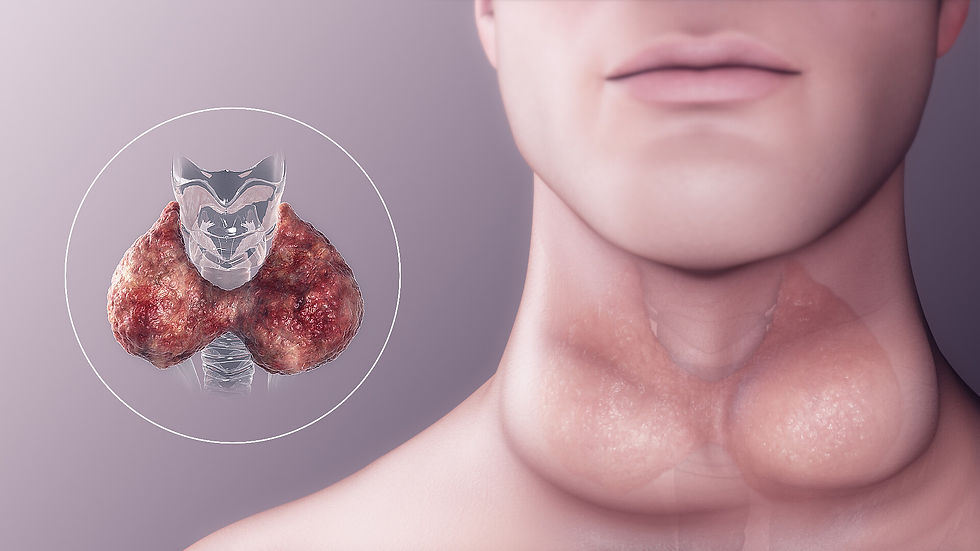
The thyroid is a small, butterfly-shaped gland in the front of the neck. Thyroid hormones control and regulate the way our body uses energy. It is responsible for providing energy to nearly every organ in the body.
Hypothyroidism is a fairly common condition. It affects approximately 2 individuals in 100. It’s prevalence increases with age, and people over 60 years old experience it more frequently. Women are more likely to have an underactive thyroid. In fact, 1 in 8 women will develop hypothyroidism.
Hypothyroidism can also affect infants and young children causing congenital hypothyroidism (previously termed endemic cretinism). It is a major cause of intellectual disability. All newborn babies are routinely screened for thyroid hormone deficiency after birth.
Symptoms may vary from one person to the other, depending on the severity of the hormone deficiency. Some people have no symptoms, while others have dramatic symptoms or rarely life-threatening symptoms. It usually starts slowly, often over a number of years. Hard to notice as it may mimic other conditions like depression.
Various organ systems may be affected by the decrease in the thyroid hormone, the most common signs and symptoms include:
- Metabolic manifestations: Cold intolerance, weight gain, hypothermia - Neurologic manifestations: Forgetfulness, paresthesia of the hands and feet - Psychiatric manifestations: Personality changes, depression, dull facial expression, dementia
- Dermatologic manifestations: Facial puffiness, coarse and dry hair and skin - Gastrointestinal manifestations: Constipation
- Cardiovascular manifestations: Slow heart rate, pericardial effusion develop slowly and rarely causes hemodynamic distress
- Other manifestations: hoarse voice, slow speech, Periorbital swelling, and occasionally there may be swelling of the front part of the neck due to goiter.
In approximately 95 percent of cases, hypothyroidism is due to a problem in the thyroid gland itself called primary hypothyroidism. Worldwide, the most common cause of primary hypothyroidism is too little iodine in the diet. Hashimoto's thyroiditis is the most common cause of hypothyroidism in countries with sufficient dietary iodine. It is an autoimmune disorder, this means the immune system starts to attack itself by making antibodies against the thyroid gland. Less common causes include treatment for an overactive thyroid gland, that may include radioactive iodine therapy, medications, or surgery.
A condition called secondary hypothyroidism can also happen. It is when the hypothalamus produces insufficient thyrotropin-releasing hormone (TRH) or the pituitary gland produces insufficient thyroid-stimulating hormone (TSH).
In the past, hypothyroidism was not diagnosed until symptoms had been present for a long time. However, simple blood tests can now detect hypothyroidism at an early stage
Laboratory testing of thyroid stimulating hormone (TSH) levels in the blood is considered the best initial test for hypothyroidism. TSH is the most sensitive test because it can be elevated even with a small decrease in thyroid function. Free thyroxine (T4), the main product of the thyroid gland, may also be measured to confirm and assess the degree of hypothyroidism. Lower-than-normal T4 levels usually mean you have hypothyroidism. However, some people may have increased TSH levels while having normal T4 levels. This is called subclinical (mild) hypothyroidism. It is believed to be an early stage of hypothyroidism. In some cases, where goiter is felt upon palpation, a thyroid ultrasound can be ordered to evaluate for any nodules (lumps) in the enlarged thyroid gland.
The goal of treatment for hypothyroidism is to return blood levels of thyroid-stimulating hormone (TSH) and thyroxine (T4) to the normal range and to relieve symptoms. Most people are treated with a synthetic long-acting form of thyroid hormone, known as levothyroxine (L-thyroxine). Blood free thyroxine(T4) and TSH levels are monitored to help determine whether the dose is adequate or not. This is done 4–8 weeks after the start of treatment or a change in levothyroxine dose. Once the adequate replacement dose has been established, the tests can be repeated after 6 and then 12 months, unless there is a change in symptoms.
